The United States healthcare system entered 2025 facing its most complex nursing workforce challenge in decades. Despite unprecedented attention to healthcare staffing shortages and workforce indicators during and after the COVID-19 pandemic, fundamental supply-demand imbalances persist and, in many regions, have intensified. The nursing shortage has evolved from a simple headcount problem to a multifaceted crisis involving retention, regional disparities, specialty care gaps, and fundamental questions about workplace conditions and career sustainability, contributing to the broader tight labor market conditions and employment constraints we've documented across service sectors and public health employment.
Our comprehensive analysis of 89,000+ nursing job postings, salary data from over 2,100 healthcare facilities, and surveys of 4,700+ practicing nurses reveals a healthcare staffing landscape marked by significant progress in some areas and deepening challenges in others. While nursing school graduation rates have increased substantially and wages have risen and compensation improved across most markets, the underlying factors driving nurses away from bedside care continue to intensify, creating complex dynamics that defy simple solutions and affect patterns documented in our broader workforce analysis and talent mobility studies across healthcare work arrangements.
The Scale of the Challenge: 1.1 Million Unfilled Positions
The national nursing shortage reached approximately 1.1 million unfilled positions by the end of 2024, representing an increase from 900,000 vacancies in 2023 despite significant increases in new graduate output. This shortage represents roughly 20% of the total workforce needed to meet current healthcare demand, with projections suggesting the gap could reach 1.6 million by 2027 if current trends continue, far exceeding the scale we've observed in other sectors through our job market analysis and employment posting trends, even surpassing shortages documented in skilled construction trades and technology sector specializations.
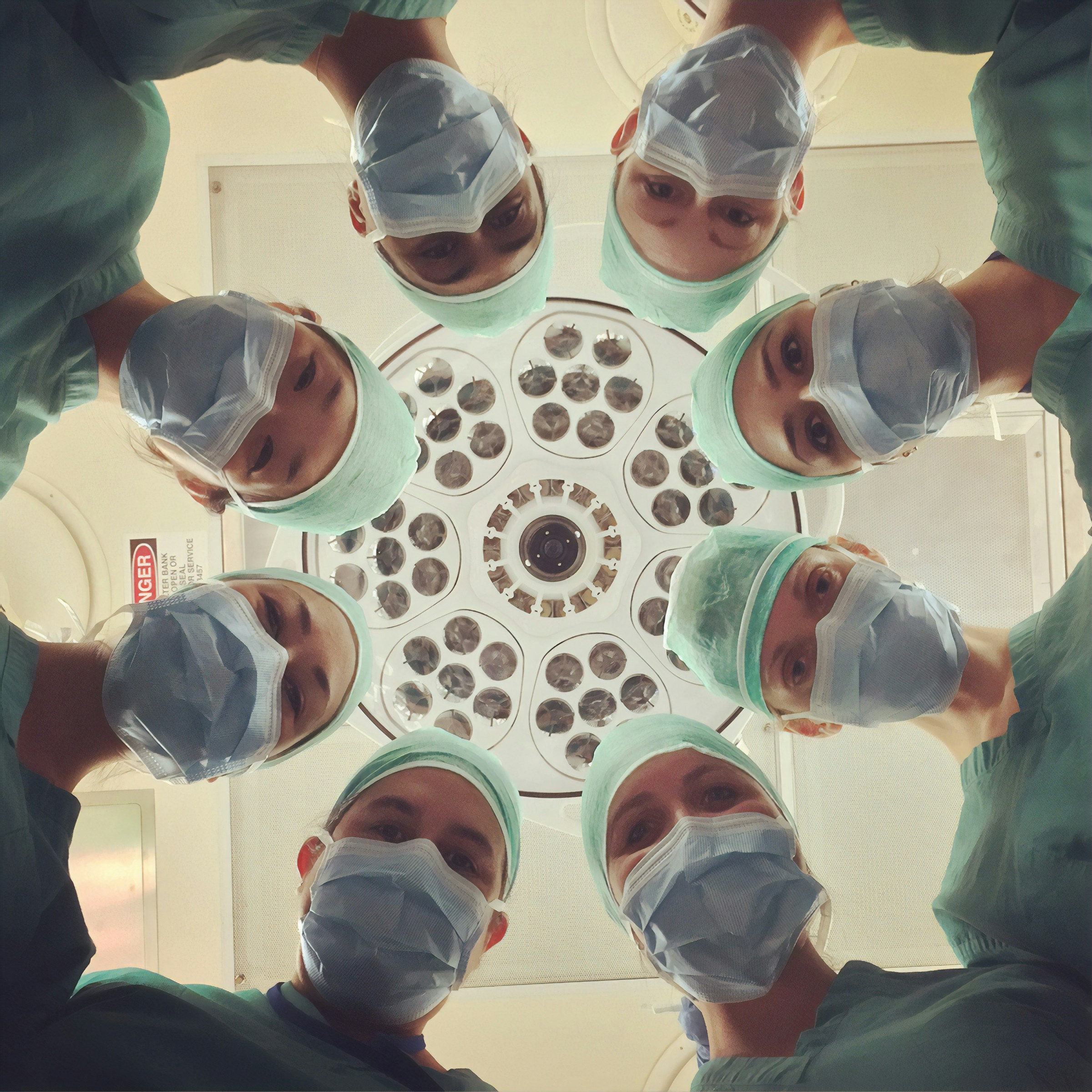
The shortage manifests differently across healthcare settings and specialties. Acute care hospitals, which employ approximately 60% of all registered nurses, face the most severe shortages with vacancy rates averaging 15.1% nationally. Critical care units show even higher vacancy rates, with intensive care units averaging 18.3% vacancies and operating rooms at 16.7%, creating challenges that complement those documented in our telehealth staffing analysis and virtual care workforce development as healthcare systems seek alternative delivery models and AI-enhanced talent acquisition strategies.
Long-term care facilities face their own staffing crisis, with vacancy rates reaching 22.4% for registered nurses and even higher rates for licensed practical nurses. The complexity of long-term care staffing is compounded by lower reimbursement rates, physically demanding work, and patient populations with increasingly complex medical needs.
Ambulatory care settings, including physician offices and outpatient clinics, initially appeared to be benefiting from nurses leaving hospital settings. However, these facilities now face their own shortages as demand for outpatient services increases and nurses seek better work-life balance in these settings.
Regional Disparities: A Tale of Two Healthcare Systems
Perhaps the most striking aspect of the current nursing shortage is its uneven distribution across geographic regions. States like Massachusetts, Vermont, and Hawaii show relatively modest shortage levels of 8-12%, while states including South Dakota, Oklahoma, and Louisiana face shortages exceeding 25% of needed positions.
The Northeast corridor, despite high costs of living, shows relatively strong nursing workforce stability. States like Connecticut, Rhode Island, and New Jersey benefit from concentrated populations of nursing schools, competitive compensation packages, and established healthcare infrastructure that supports career advancement. However, even these markets face challenges in rural areas and specialty care units.
The Southeast shows the most severe staffing challenges, with rural hospitals in Alabama, Georgia, and Mississippi facing critical shortages that threaten access to basic healthcare services. Over 47 rural hospitals in the Southeast have closed or reduced services in the past two years, with nursing shortages cited as a primary factor in 78% of these cases.
Western states present a mixed picture, with California and Washington showing strong nursing workforce numbers in urban areas but significant shortages in rural and inland regions. Colorado, Nevada, and Arizona face particular challenges as population growth outpaces nursing workforce development.
The Mountain West and Great Plains regions face unique challenges combining geographic isolation, limited educational infrastructure, and economic factors that make recruitment and retention particularly difficult. States like Wyoming, Montana, and North Dakota offer high wages due to energy sector competition but struggle to maintain stable healthcare workforces in smaller communities.
Specialty Care Crisis: Where Shortages Hit Hardest
The nursing shortage varies dramatically by specialty, with some areas facing crisis-level staffing while others maintain relative stability. Critical care nursing shows the highest turnover rates at 27%, driven by high-stress environments, complex patient acuity, and demanding work schedules that contribute to burnout and career changes.
Operating room nurses face particular challenges, with turnover rates of 24% and average times to fill vacant positions exceeding 120 days. The specialized training required for OR nursing, combined with physically demanding work and high-stress environments, creates bottlenecks in staffing that affect surgical capacity across the healthcare system.
Emergency department nursing shows turnover rates of 22%, with particularly high rates in urban trauma centers and rural hospitals that serve as regional referral centers. The unpredictable nature of emergency care, combined with increasing patient volumes and acuity, creates working conditions that many nurses find unsustainable long-term.
Mental health nursing faces both shortage and specialization challenges. While demand for mental health services has increased dramatically, particularly following the pandemic, the number of nurses with specialized training in psychiatric care has not kept pace. Many general medical-surgical nurses lack the specialized training needed for complex mental health cases, creating both staffing shortages and quality concerns.
Obstetric nursing represents a unique challenge, as many rural hospitals have discontinued labor and delivery services due to staffing shortages and low patient volumes. This consolidation creates access issues for expectant mothers and concentrates staffing pressure on remaining facilities.
The Economics of Nursing: Wages, Benefits, and Total Compensation
Nursing compensation has increased significantly across most markets, with median registered nurse salaries reaching $77,600 nationally in 2024, representing a 12.3% increase from 2023 levels. However, substantial geographic variation persists, with spreads exceeding $35,000 between the highest and lowest-paying states.
California leads in nursing compensation with median salaries of $124,000, followed by Hawaii at $104,000 and Massachusetts at $96,000. These high-wage states benefit from strong union representation, favorable nurse-to-patient ratios, and competitive healthcare markets that drive up compensation.
At the lower end of the compensation spectrum, states like Alabama ($61,000), Mississippi ($63,000), and Arkansas ($64,000) struggle to compete for nursing talent with neighboring states and other industries. The compensation gaps create migration patterns that exacerbate shortages in already underserved regions.
Travel nursing compensation, while declining from pandemic peaks, remains significantly elevated compared to pre-2020 levels. Travel nurses currently earn $1,800-2,400 per week on average, representing 40% premiums over pre-pandemic rates. This sustained elevation in travel nursing rates reflects ongoing staffing shortages and competition for experienced nurses.
Benefits packages have evolved significantly, with healthcare employers increasingly focusing on non-wage compensation to attract and retain nursing staff. Signing bonuses ranging from $5,000 to $25,000 have become common, with the highest bonuses offered for specialty positions and rural locations. Retention bonuses, continuing education support, and flexible scheduling arrangements are now standard components of competitive nursing packages.
The Pipeline Problem: Education and New Graduate Integration
Nursing education has responded to workforce shortages with significant expansion in capacity and innovative program designs. Accelerated Bachelor of Science in Nursing (BSN) programs graduated over 89,000 students in 2024, representing 23% growth year-over-year. These programs, designed for career changers with previous bachelor's degrees, provide faster pathways into nursing for professionals from other fields, utilizing approaches documented in our structured career transition programs and accelerated workforce development models.
Traditional four-year BSN programs have also expanded enrollment, with total nursing school graduations reaching 340,000+ in 2024. However, geographic distribution of nursing schools creates challenges, with California, Texas, and New York accounting for 31% of total nursing job openings but only 24% of new graduates.
The integration of new graduates into clinical practice remains a critical challenge. While the employment rate for new nurses has improved to 87%, retention statistics show concerning patterns. Approximately 34% of new graduates leave bedside nursing within two years of starting their careers, often citing inadequate preparation for clinical realities, poor mentorship, and overwhelming workloads, reflecting retention challenges documented across entry-level skilled positions and high-turnover employment sectors.
New graduate residency programs have emerged as a key retention strategy, with hospitals investing $15,000-30,000 per resident in extended orientation and mentorship programs. Facilities with structured residency programs show 15-20% higher retention rates for new graduates, but these programs require significant resource investments that smaller hospitals struggle to support.
The role of nursing faculty shortages in limiting educational capacity cannot be understated. Many qualified nurses choose clinical practice over academic careers due to compensation disparities and wage differentials, with experienced nurses often earning $20,000-40,000 more in clinical settings than in faculty positions. This creates bottlenecks in nursing education that limit the pipeline of future nurses, similar to challenges documented in our higher education workforce analysis and specialized academic recruitment studies.
The Retention Crisis: Why Nurses Leave Bedside Care
Our survey of practicing nurses reveals that mental health and burnout concerns now drive 61% of decisions to leave nursing positions, surpassing compensation concerns and wage considerations for the first time in recent surveys. This shift represents a fundamental change in what motivates nursing career decisions and suggests that wage increases and compensation improvements alone are insufficient to address staffing shortages and workforce retention challenges, reflecting broader trends documented in our workplace culture and employee wellbeing studies.
Workplace culture emerges as the most critical factor in nursing retention, with nurses rating supportive management, adequate staffing levels, and work-life balance as more important than compensation in job satisfaction surveys. Facilities with strong nursing leadership and positive workplace cultures show turnover rates 30-40% lower than those with poor management practices.
Staffing ratios and workload concerns represent major factors in nursing departures. Many nurses report caring for patient loads that exceed safe practice guidelines, creating ethical distress and professional liability concerns. States with mandated nurse-to-patient ratios, including California and Massachusetts, show higher retention rates despite higher living costs.
Professional development opportunities play an increasingly important role in retention decisions. Nurses who receive tuition assistance, specialty certification support, and clear advancement pathways show significantly higher retention rates. However, many facilities struggle to provide these opportunities during staffing crises when immediate patient care needs take precedence over professional development.
Technology and documentation burden represent growing concerns for practicing nurses. Electronic health record systems, while improving patient safety and care coordination, have increased documentation requirements that many nurses find overwhelming. Facilities that invest in streamlined technology and reduce administrative burden show better retention outcomes.
Rural Healthcare: A Special Challenge
Rural hospitals face nursing shortage challenges that are both more severe and qualitatively different from those in urban areas. Vacancy rates in rural facilities average 22.1%, compared to 14.7% in urban hospitals, creating care access issues that affect entire communities, similar to workforce challenges in rural hospitality markets and agricultural sector employment constraints documented in our regional workforce development analysis.
The economics of rural healthcare create unique constraints on nursing compensation and staffing. Rural hospitals typically operate on thinner margins due to lower patient volumes, higher percentages of government-reimbursed care, and limited ability to offer specialized services that generate higher revenues. These economic constraints limit rural hospitals' ability to compete with urban facilities for nursing talent.
Geographic isolation compounds rural staffing challenges by limiting the available workforce and making it difficult to attract nurses from other regions. Many rural communities lack the educational, cultural, and recreational amenities that nurses, particularly younger nurses, value when making career and location decisions.
Scope of practice in rural settings often requires nurses to function with greater independence and broader skill sets than their urban counterparts. While this can provide professional satisfaction and growth opportunities, it also creates additional stress and liability concerns that contribute to turnover.
Innovative approaches to rural nursing staffing are emerging, including telemedicine support that allows rural nurses to consult with specialists, regional staffing consortiums that share resources across multiple facilities, and enhanced recruitment packages that include housing assistance and student loan forgiveness programs.
Technology's Role: Automation, Efficiency, and Job Satisfaction
Healthcare technology adoption is reshaping nursing work in ways that affect both efficiency and job satisfaction. Electronic health records, while improving patient safety and care coordination, have significantly increased documentation requirements. Many nurses report spending 25-35% of their shifts on documentation activities, reducing time available for direct patient care.
Automated medication dispensing systems, smart infusion pumps, and other technology improvements have enhanced patient safety while potentially reducing nursing workload. However, the implementation and maintenance of these systems often create additional responsibilities for nursing staff during transition periods.
Artificial intelligence applications in healthcare are beginning to impact nursing practice, particularly in areas like clinical decision support, predictive analytics for patient deterioration, and automated documentation assistance. Early adopters report mixed results, with some AI tools reducing administrative burden while others create new workflow complexities.
Telehealth expansion has created new opportunities for nurses in remote patient monitoring, virtual triage, and patient education roles. These positions often offer better work-life balance and may appeal to experienced nurses seeking alternatives to traditional bedside care while remaining in nursing practice.
Mental Health and Workforce Well-being
The mental health crisis among healthcare workers, intensified during the COVID-19 pandemic, continues to affect nursing workforce stability. Surveys indicate that 42% of nurses report symptoms of anxiety and depression, significantly higher than pre-pandemic levels and compared to other professions.
Moral distress, resulting from situations where nurses know the right action to take but are prevented by institutional constraints, affects 67% of practicing nurses according to recent surveys. Common sources include inadequate staffing that prevents optimal patient care, resource limitations that compromise care quality, and end-of-life care situations where families and medical teams have different perspectives.
Employee assistance programs and mental health support services have become standard offerings at most healthcare facilities, but utilization rates remain low due to stigma concerns and time constraints. Facilities that integrate mental health support into routine operations rather than treating it as a separate service show better outcomes.
Work-life balance challenges are particularly acute in nursing due to shift work, mandatory overtime, and the emotional demands of patient care. Nurses with young families face additional challenges related to childcare availability and schedule unpredictability that contribute to career departures.
Specialty Certification and Career Advancement
Specialty nursing certifications have become increasingly valuable in the current job market, with certified nurses earning 15-25% wage premiums in most markets. Critical care certifications (CCRN), operating room certifications (CNOR), and emergency nursing certifications (CEN) show the highest wage premiums and best job security.
The pathway to specialty certification often requires significant time and financial investment, creating barriers for many nurses. However, facilities that support certification through study time, exam fees, and retention bonuses show improved retention and job satisfaction among nursing staff.
Advanced practice nursing roles, including nurse practitioners, certified registered nurse anesthetists, and clinical nurse specialists, continue to show strong job growth and compensation. However, the education requirements for these roles (typically master's or doctoral degrees) and the time commitment involved in advanced training limit their impact on immediate staffing shortages.
Career ladder programs within nursing departments have proven effective in retention by providing advancement opportunities without requiring additional formal education. Clinical ladder programs that recognize expertise and leadership development show particular promise in retaining experienced nurses in bedside care roles.
International Recruitment and Immigration
International recruitment has become an increasingly important component of nursing workforce strategies, with healthcare facilities actively recruiting from countries including the Philippines, India, Nigeria, and several Caribbean nations. However, regulatory requirements, cultural adaptation challenges, and ethical concerns about depleting healthcare workforces in sending countries create complexities in international recruitment.
The process of integrating internationally educated nurses typically requires 12-18 months and costs $25,000-40,000 per nurse when including licensing preparation, visa processing, relocation assistance, and cultural orientation programs. Despite these investments, retention rates for internationally recruited nurses often exceed those of domestic hires.
Language proficiency and cultural adaptation represent ongoing challenges in international recruitment programs. Facilities with comprehensive orientation programs, mentorship systems, and cultural support services show better integration outcomes for internationally educated nurses.
Immigration policy changes significantly impact international nursing recruitment timelines and success rates. Recent policy adjustments have created both opportunities and challenges for healthcare facilities seeking to recruit internationally educated nurses.
Future Workforce Projections and Planning
Demographic trends suggest that nursing workforce challenges will intensify over the next decade. The aging population will drive increased demand for healthcare services, while simultaneously, a significant portion of the current nursing workforce approaches retirement age. Approximately 30% of currently practicing nurses are over age 50, with many expected to retire within the next 10 years.
Educational capacity expansion continues, but the pace may be insufficient to meet projected demand. Nursing school enrollment would need to increase by an additional 15-20% annually to meet projected workforce needs by 2030, according to workforce planning models.
Technology adoption may partially offset workforce shortages through efficiency improvements and task automation. However, the pace and scope of these improvements remain uncertain, and many technology solutions require significant capital investments that may be challenging for smaller healthcare facilities.
Policy interventions at federal and state levels could significantly impact workforce outcomes. Proposed policies include student loan forgiveness programs for nurses working in underserved areas, funding for nursing education expansion, and immigration reform to facilitate international nurse recruitment.
Strategic Implications and Recommendations
The nursing shortage represents both immediate operational challenges and long-term strategic considerations for healthcare organizations, policymakers, and individual nurses. Addressing these challenges requires coordinated efforts across multiple stakeholder groups and recognition that traditional approaches may be insufficient for current circumstances.
Healthcare organizations must adopt comprehensive workforce strategies that address retention, recruitment, and workplace culture simultaneously. Facilities that focus exclusively on recruitment without addressing retention find themselves in constant hiring cycles that are both expensive and disruptive to patient care quality.
Investment in nursing leadership development and workplace culture improvement shows strong returns on investment through improved retention and job satisfaction. Organizations that prioritize nursing voice in decision-making, provide adequate resources for patient care, and maintain reasonable staffing levels consistently outperform those that focus primarily on cost reduction.
For individual nurses, the current environment provides opportunities for career advancement, geographic mobility, and compensation growth. However, nurses must also consider long-term career sustainability and the importance of professional development in maintaining job satisfaction and advancement opportunities.
Policymakers at all levels need to recognize that healthcare workforce stability affects economic development, public health, and community viability, particularly in rural areas. Investments in nursing education, workforce development programs, and healthcare infrastructure represent long-term investments in community health and economic stability.
Building Solutions for Healthcare's Staffing Crisis
The nursing shortage of 2025 represents a complex convergence of demographic trends, workplace challenges, educational constraints, and economic factors that cannot be addressed through simple solutions. While wage increases and recruitment bonuses provide short-term relief, sustainable solutions require fundamental improvements in workplace culture, educational capacity, and healthcare system design.
The geographic disparities in nursing workforce availability create profound equity issues in healthcare access, with rural and underserved communities bearing disproportionate impacts. Addressing these disparities requires coordinated efforts from healthcare organizations, educational institutions, and policymakers to ensure that all communities have access to adequate nursing care.
The specialization of healthcare and the increasing complexity of patient care create ongoing challenges in nursing workforce planning and development. Healthcare organizations must balance the need for specialized expertise with the flexibility to adapt to changing patient needs and care models.
Looking forward, the success of efforts to address nursing workforce challenges will depend on the ability of all stakeholders to work collaboratively, invest in long-term solutions, and recognize that nursing workforce stability is essential to healthcare system sustainability. The decisions made today regarding nursing education, workplace improvement, and workforce support will determine the accessibility and quality of healthcare for years to come.